11 Heartwarming Stories Proving Kindness Is a True Superpower

In a groundbreaking revelation for maternal mental health, a new study suggests that postpartum depression may actually begin long before childbirth. For expectant mothers, this discovery offers not only a deeper understanding but also a sense of hope — the chance to identify and address the condition before it fully emerges.
The content provided is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified healthcare provider with any questions you may have regarding a medical condition.

For years, postpartum depression was often dismissed as a brief emotional phase, but it is, in fact, a serious medical condition that affects about 1 in 7 women. It can profoundly impact a mother’s mental health, her connection with her baby, and the overall family dynamic. Up to 5% of women report persistently high levels of depressive symptoms even three years after giving birth.
Its symptoms may include persistent sadness, frequent crying, loss of interest or pleasure, changes in appetite, fatigue, irritability, anxiety, poor sleep, and overwhelming feelings of guilt or hopelessness.
While it was once believed to occur only in the weeks after childbirth — triggered by exhaustion, hormonal shifts, and lack of sleep — new research shows that changes in the brain may begin during pregnancy itself, potentially setting the stage for mood disorders before the baby is even born.
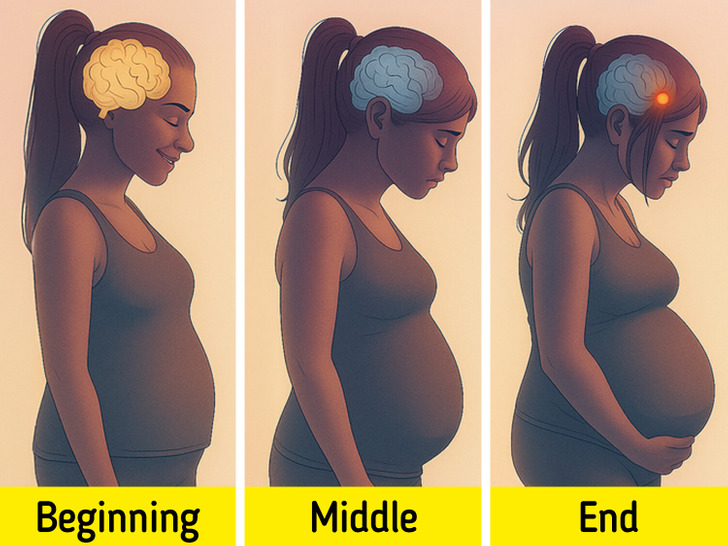
A new study analyzed brain images of 118 women — 88 pregnant and 30 non-pregnant — during the third trimester and after delivery. What they found was both revealing and disturbing: specific structural changes in key brain regions before the baby was born.
Notably, researchers found an increase in the volume of the amygdala — a brain region involved in emotion processing and stress response — in women who later developed symptoms of postpartum depression. Changes were also detected in the hippocampus, a structure responsible for memory and emotional regulation, particularly among those who experienced more traumatic births or elevated stress levels.
These findings suggest that the neurological “signature” of postpartum depression may emerge well before childbirth, challenging the traditional view that the condition develops only after the baby is born.

One of the most hopeful revelations of the study is the possibility that these transformations may be detectable by neuroimaging before delivery. In other words, we could anticipate the onset of postpartum depression with specific clinical tools, such as brain MRI scans.
This opens a new window in preventive medicine: if we identify early neurobiological markers, it is possible to offer personalized interventions to the most vulnerable mothers-to-be — from psychological support to hormonal regulation — before symptoms set in.
In addition, researchers are studying biomarkers in the blood in order to develop a blood test that measures the levels of the neurosteroids to estimate a person’s risk of PPD.

Postpartum depression affects far more than just the mother — it can hinder a baby’s emotional and social development. When a mother feels overwhelmed or emotionally distant, her ability to form a secure bond with her child may weaken, disrupting that vital early connection that supports healthy growth. Research also shows that children raised by mothers with chronic depression tend to score lower, on average, on cognitive, emotional, and behavioral assessments.
These findings reach beyond medicine — they carry deep social and cultural implications. Investing in perinatal mental health is not a privilege but a necessity. Motherhood begins in the body, but it also takes shape in the brain — and every transformation deserves support, care, and understanding.
Much remains to be discovered: why some women develop symptoms and others do not, exactly how long post-pregnancy brain changes last (some studies indicate that they may extend for more than two years), or how factors such as prior psychiatric history and social context influence the equation.
What is clear is that we are facing a paradigm shift. The neurobiology of childbearing is not static, uniform, or easily predictable, but it can be understood and addressed with increasingly sophisticated scientific tools. And that is excellent news.
For years, postpartum depression was seen merely as an emotional response to the difficulties of new motherhood. But modern research reveals a far more complex picture — one that starts long before childbirth and is rooted deep within the brain’s structure and chemistry. This understanding not only helps lift the burden of guilt from women who struggle “without reason,” but also paves the way for more accurate diagnoses and genuinely compassionate care.
Be sure to check out our other article featuring celebrity moms who are challenging the stigma surrounding breastfeeding.