12 Nannies Whose Babysitting Experiences Could Rival a Blockbuster Plot
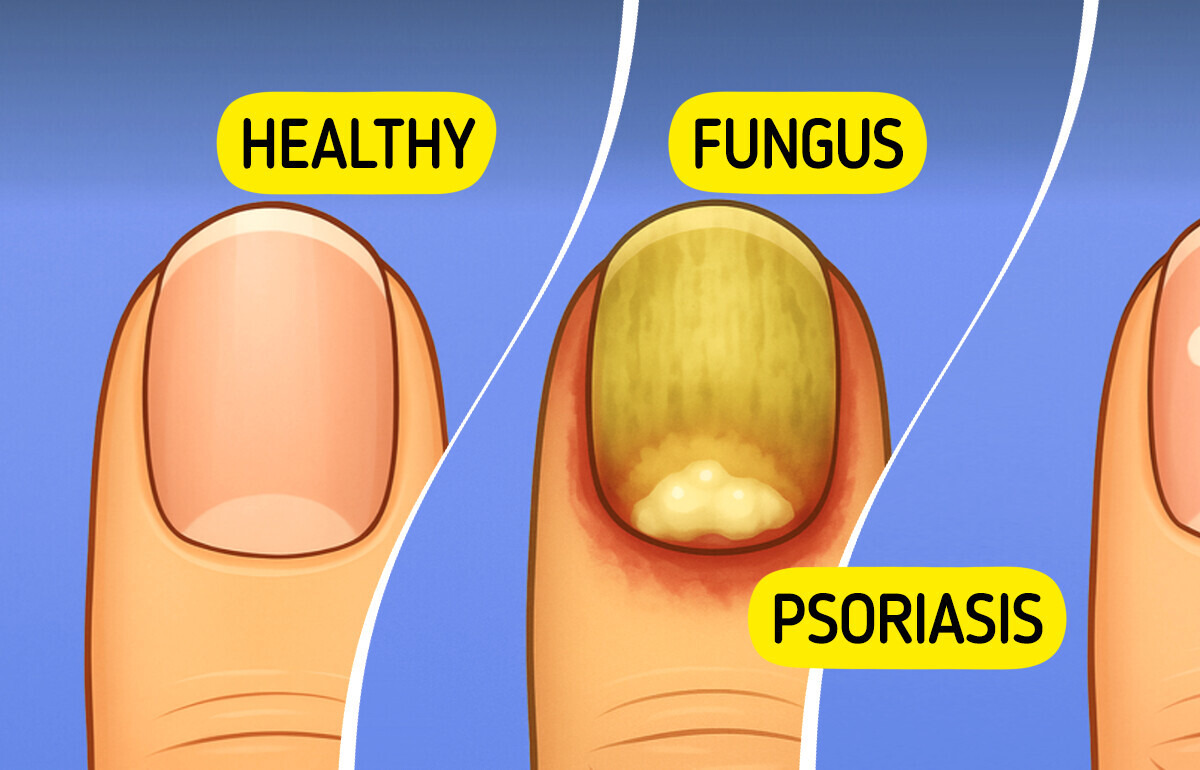
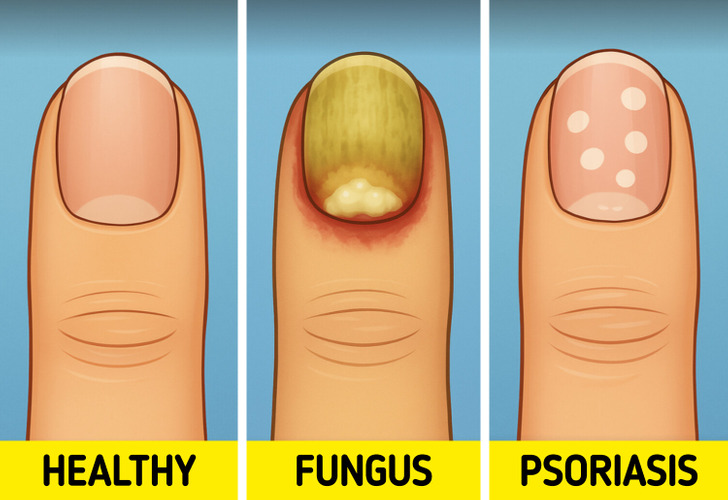
Psoriasis isn’t just about what shows up on your skin. Beneath every flare-up, there are hidden triggers quietly working against you — some you’d never even think to blame. Here’s what you need to know to spot them before your next flare strikes.
CONTENT IS PROVIDED FOR INFORMATIONAL PURPOSES ONLY AND IS NOT INTENDED AS A SUBSTITUTE OF MEDICAL ADVICE.
SEEK GUIDANCE OF YOUR DOCTOR REGARDING YOUR HEALTH AND MEDICAL CONDITIONS.
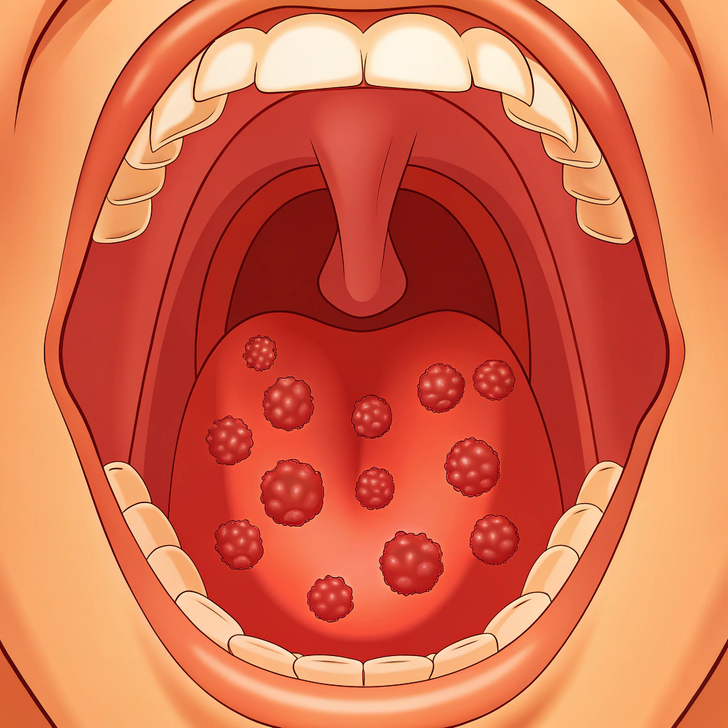
Did you know that a sore throat can make psoriasis worse?
In a study of 275 people with psoriasis, 42% said their skin flared up after a sore throat — and that number rose to 72% if it was caused by strep. Women and people who got psoriasis at a young age were even more likely to have flare-ups.
Surprisingly, nearly half of the people who had their tonsils removed saw their psoriasis improve. This suggests tonsil removal might help some patients.

Not getting enough quality sleep can increase inflammation in the body and disrupt immune function, which may worsen psoriasis. Studies show that poor sleep is linked to increased psoriasis severity, creating a vicious cycle: the itch keeps you up, and lack of sleep triggers more flares.
Prioritizing a regular sleep schedule, reducing screen time before bed, and managing nighttime itching can help break this cycle.

Every time you work out, you might sweat a lot — and that’s when the trouble starts. The sweat makes your skin itch like crazy. You scratch it, sometimes so hard that you break the skin, and it starts to bleed.
The result? Painful, inflamed skin that leaves you regretting giving in to the itch — even if it felt good for a moment.

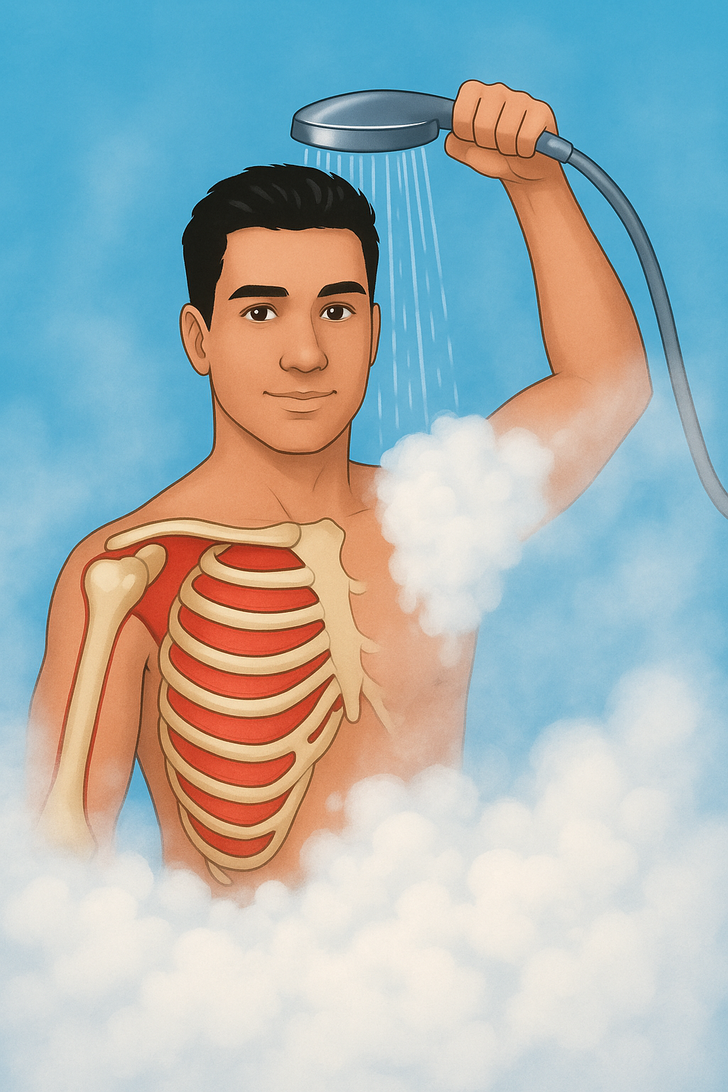
Steaming hot showers may feel amazing, but they can be tough on psoriasis-prone skin. The heat dries out the skin, leaving it white, flaky, and more vulnerable to flare-ups. The hotter and longer the shower, the higher the risk.
For many, showers are more than just hygiene — they’re a way to cope with stress, anxiety, and depression. Sometimes, that can mean multiple showers a day, which may make symptoms worse.
To protect the skin, lukewarm showers are the best option. When anxiety leads to frequent showers, it might help to explore other calming techniques, like meditation, deep breathing, exercise, or journaling. Finding what works best can make a big difference.
Allergies to certain skincare products, fragrances, or detergents can irritate the skin, making it more likely to develop plaques through the Koebner response. Even contact with nickel in jewelry or certain fabrics can lead to irritation that sparks a flare-up.
Switching to fragrance-free, hypoallergenic products and wearing soft, breathable clothing can help reduce this risk.

Hormonal shifts, especially in women, may affect psoriasis. Flare-ups often happen during puberty or menopause, when hormone levels change.

Cuts, scrapes, insect bites, or sunburns can cause psoriasis flare-ups. This reaction is known as the Koebner response.

Cold or dry climates can dry out the skin, often leading to psoriasis flare-ups.