18 People Who Truly Know What It Means to Be Unlucky


Have you ever looked down at your toenails and thought something seemed off? Most of us don’t pay them much attention until something changes. Maybe they turn yellow, feel thicker than usual, or show odd ridges or spots you hadn’t noticed before.
Here’s a simple guide to five common toenail changes, what they could mean, and how to tell when a home remedy might be enough—or when it’s smarter to check in with a doctor.
Medical disclaimer: This article is for general information only and should never replace personal advice from a qualified healthcare provider. If you spot any of the changes below—or anything else that worries you—book a doctor’s visit for a proper diagnosis and treatment plan.
If your toenails start to look like old parchment—thick, cloudy, and tinted yellow or light brown—there’s a good chance you’re dealing with a fungal infection called onychomycosis. As the fungus settles in, the nail might become brittle, start to split, or even lift away from the nail bed entirely.

When the toe box keeps hitting or squeezing the nail plate, two things happen:
If your nail plate dips in the middle enough to hold a drop of water, you’re looking at koilonychia (spoon nails). They often feel thin or crack easily.

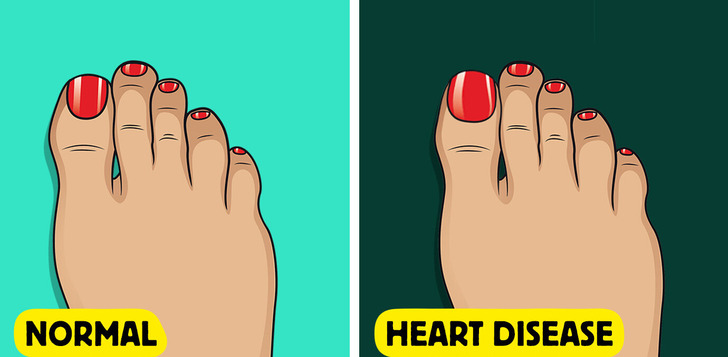
A dusky, blue-gray nail bed screams cyanosis—a sign your extremities aren’t getting enough oxygenated blood.
If you’re constantly dealing with ingrown toenails that just won’t heal—even when you’re trimming them correctly—it could be a sign of something deeper going on, like poor circulation or diabetic nerve damage.
When the edge of your toenail starts digging into the skin beside it, the area can get red, swollen, and even a little oozy. Yep—that’s an ingrown toenail making itself known.

A nail that appears dusted with white powder—often rough, brittle, and easy to scrape—signals white superficial onychomycosis (WSO), a variant of nail fungus in which dermatophytes invade only the topmost keratin layers. Because the infection sits superficially, it seldom hurts and responds well to mechanical filing plus topical antifungals; oral tablets are reserved for stubborn or extensive disease. Dermatologists differentiate WSO from “true” leukonychia (harmless white lines that arise in the nail matrix) by gently paring the surface: fungal chalk comes off as powder, whereas leukonychia is built into the plate. Untreated WSO can, however, spread deeper or to other toes, so confirming the organism with a KOH prep or PCR before treatment remains best practice.
If you have onychomycosis (nail fungus) along with burning or numb toes, it’s crucial to consider underlying health issues like diabetes or peripheral vascular disease (PVD). High blood sugar levels significantly impair blood flow and weaken the immune system. This makes it harder for your body to fight off the fungal infection, leading to persistent nail fungus and an increased risk of developing painful ulcers.

A nail that turns jet‑black or develops a coal‑coloured patch is most often hiding blood—a subungual haematoma that forms after a knock, a long hike or miles in tight running shoes. The pooled blood stays trapped beneath the plate, explaining the throbbing pain many people feel and the way the stain “grows out” with the nail over weeks. Yet dermatologists are equally alert for the other major cause of black pigment: subungual melanoma, a rare form of skin cancer. Unlike a bruise, melanoma usually begins as a thin brown‑to‑black stripe on a single nail, then slowly widens or spills onto the cuticle (Hutchinson’s sign). Any dark band that enlarges, varies in colour, or appears without remembered trauma deserves same‑week review, because outcome hinges on early excision.
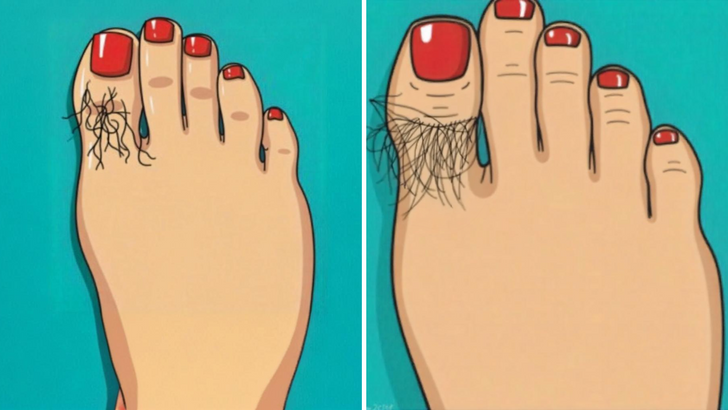
Don’t dismiss those wispy toe hairs! They’re more than just cosmetic; they act as a free, early warning system for your foot’s circulatory health. Healthy blood flow keeps those hair follicles active. If you experience sudden, unexplained toe or foot hair loss, it could be an early sign of peripheral arterial disease (PAD). PAD is a condition where plaque buildup restricts blood flow, depriving tissues of vital oxygen. This hair loss serves as a crucial indicator to seek medical attention.
Your toenails might be trying to tell you something, but they’re not the only messengers. If you’ve been feeling off lately in ways you can’t quite explain, your body might be waving another red flag. Up next: could gluten be the real culprit?